Dupree Johnson was 9 when he first started abusing drugs and alcohol.
For two decades, Johnson was deep in his addiction. He had no plans to change his ways.
“I used to beg for change out front of McDonald's. I was homeless. And I wasn't trying to get change to eat,” he said. “Heroin was always in the picture. I was kind of like a garbage can – I'd use whatever was there.”
If you or someone you know is struggling with addiction and substance abuse, go to helpisherede.com or call 800-345-6785.
In high school, Johnson played football at a Washington, D.C.-area school and had about nine teammates who “started dipping and dabbling into drugs and selling drugs,” he said.
As the years went by, Johnson shifted from dealing to using. Teammates began to die, one by one.
“They were either being killed on the streets or by overdoses,” he said. As he became an adult, he realized it was down to two men: Himself and a former teammate serving 25-to-life in prison.
“So I was the only one left, and one day it just hit me that I really need to get my life together,” he said. Warwick Manor treatment center brought Johnson to the Eastern Shore, where he began his recovery and eventually re-entered the workforce. After less than a year working a job that helped him buy a car and rent a nice apartment in Salisbury, Md., Johnson realized he was meant to do more than sell cell phones. He quit his high-paying management job, started working for Warwick at minimum wage and later found an invite to work and receive further education to become a counselor at Sussex County Correctional Institution.
As the years went by, Johnson worked with dozens of criminals struggling with substance abuse like he had. But when he realized he was treating the children of offenders he had once worked with, he decided enough was enough.
“I'll never forget it when [another counselor] said, 'You can catch them in the high chair stage or you can catch them in the electric chair stage. That's up to you, but you need to do the work,'” Johnson said.
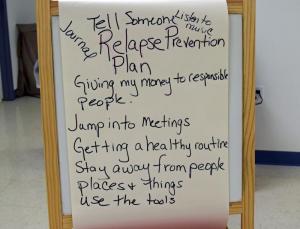
Now, after about eight years of being clean, with healed gunshot wounds to remind him of his past, he's focusing on prevention, both to prevent himself from relapsing and to prevent at-risk children and teens from turning to drugs.
“It's not that we don't have enough treatment,” he said. “We don't have enough prevention. Prevention is the key. Even when a person goes through treatment and they finish their treatment cycle, they have to go back to prevention to prevent themselves from relapsing.”
Johnson now lives in Lincoln and works as a prevention program manager at Kent Sussex Community Services and is a facilitator of the Sussex County Action Prevention Coalition, a branch of the Kent Sussex Action Prevention Coalition, which is a collection of health providers, civic and community groups and state resources that formed in summer 2011 to raise awareness and improve education about substance abuse and addiction.
“It's not really about the drugs,” he said. “Addiction is about having behaviors that center around compulsion, obsession and self-centeredness. That addiction can be to anything, not just drugs. Drugs are just a symptom. It's like a sneeze or a cough is to the flu.”
State funding to bring more beds
In the past three years, Delaware legislators have responded to the heroin epidemic by adding $8 million for substance-abuse services, said Department of Health and Social Services Secretary Rita Landgraf.
In the current fiscal year ending June 30, $4.5 million of that additional funding will cover some of the costs associated with the new Harrington detox center, as well as the expansion of treatment beds. An additional $3 million proposed in the fiscal year 2017 budget will fund new programs, including housing vouchers, expansion of partial-hospitalization programs and a planned substance use disorder assertive community treatment team, a collaboration of health and community service professionals that will help a limited number of recovering addicts get back on their feet.
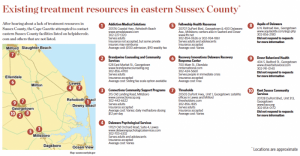
Outpatient options in eastern Sussex County
After hearing about a lack of treatment resources in Sussex County, the Cape Gazette attempted to contact eastern Sussex County facilities listed on helpisherede.com and others that are not listed.
Addiction Medical Solutions
20576 Coastal Hwy., Rehoboth Beach
302-227-1320
Serves adults
Insurance not accepted, but some private insurers may reimburse
Average cost: $100 admission, $90 weekly fee
Brandywine Counseling and Community Services
528 East Market St., Georgetown
302-856-4700
Serves adults
Insurance accepted
Average cost: Sliding fee scale option available
Connections Community Support Programs Inc.
1 East St., Harrington; 315 Old Landing Road, Millsboro
302-442-6622
Serves adults
Insurance accepted
Average cost: Varies; daily methadone dosing $12 per day
Delaware Psychological Services
17021 Old Orchard Road, Suite 4, Lewes
www.delawarepsychologicalservices.com
302-703-6332
Serves adults and adolescents
Insurance accepted
Average cost: Varies
Fellowship Health Resources
20707 DuPont Blvd., Georgetown and 400 Delaware Ave., Suite 105, Millsboro; centers also in Seaford and Dover
302-854-0626 or 302-934-1861
Serves adults and adolescents
Insurance accepted
Average cost: Varies
Recovery Innovations Delaware Recovery Response Center
700 Main St., Ellendale
302-424-5660
Serves people in immediate crisis
Insurance accepted
Average cost: Free
Thresholds
20505 DuPont Hwy., Unit 1, Georgetown; satellite offices in Lewes and Milford
302-856-1835
Serves adults
Insurance accepted
Average cost: Varies
The following facilities did not respond to multiple requests for more information:
Aquila of Delaware
6 N. Railroad Ave., Georgetown
302-856-2180
Dover Behavioral Health
404 S. Bedford St., Georgetown
302-741-0140
Kent Sussex Community Services
20728 DuPont Blvd., Unit 313, Georgetown
302-854-0172
State funding also will support more inpatient treatment beds and sober-living facilities throughout the state, increasing the total number of statewide beds from 78 to 95. The new sober-living facilities, where addicts who have already detoxed can live in a structured, drug-free environment, will double bed availability statewide from 60 to 120.
However, all three new, 16-bed residential treatment facilities are planned for New Castle and Kent counties, with two operating in Smyrna and one in Wilmington. The only facility on the horizon for Sussex County is a 16-bed residential treatment center in Ellendale for young adults ages 18 to 25 who have co-occurring mental health and substance abuse disorders, which will be operated by Pennsylvania-based Gaudenzia. State officials said the Ellendale facility should be online this year.
In Sussex County, the only other planned residential treatment center is a behavioral health hospital in Georgetown, run by the for-profit SUN Behavioral Health and slated to open in 2017.
The 90-bed facility will have a wing for detox and substance abuse treatment, but specific treatment programs have not yet been made public.
Community support needed for lifelong recovery
State health department officials say there are plans to open more than a dozen sober-living facilities, but only two will be located in Sussex County, providing about 22 beds for people who have already gone through initial treatment.
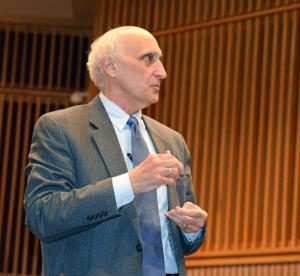
Dr. Michael Barbieri, a former state representative who is now the director of the state Division of Substance Abuse and Mental Health, said at a recent meeting in Seaford that as the state adds new treatment options and he hones in on properly placing those resources in the communities that need them most, Sussex County residents need to show support.
“I need you to advocate for these services, because quite honestly, every time we try to place services somewhere, people say, 'Not in my backyard. We need it, we want it, but not here,'” he said. “We have to really let people know that people who are struggling with an addiction, people that are struggling with mental illness, are good, community people. They're like all of us. They are us.”
Barbieri said the state lacks what he refers to as a “soft” or “warm” hand-off, meaning that when addicts go to the emergency room for an overdose or drug-related illness or injury, they should be connected to treatment resources as they're walking out the door. Or when an addict goes through detoxification, the patient should be directed to a continuum of care that includes outpatient services, counseling, therapy and sober living arrangements as they work on their recovery.
Community support groups, such as Alcoholics Anonymous, Narcotics Anonymous and aTAcK Addiction, also play a vital role in the recovery process and in an addict's ability to reconnect with their community, family and friends.
Barbieri said the state must get away from a system of maintaining addictions, and instead develop strategies toward long-term recovery.
Barbieri said the current system just maintains people struggling with substance abuse.
“We don't want to do that any longer,” he said. “We want them to be able to thrive. We want them to be able to live in a community and be successful in that community.”
Money for more treatment options is necessary, but it's not the entire answer, said Peggy Geisler, executive director of the Sussex County Health Coalition.
“There's never going to be enough money to put the perfect system in place,” Geisler said. "We absolutely don't have all the answers, but we want to roll our sleeves up and be part of the solution in a smart way."
But there is no overnight, miracle cure.
“There's a lot of fear, frustration and pain from the personal loss, and often we want to hurry up and fix it," she said. "People ask, 'Isn't there something I can do immediately?' Of course there are things each one of us personally can do.”
Mentoring at-risk children through community programs, volunteering at homeless shelters or soup kitchens or going to the local hospital to rock drug-exposed babies are just a few options for people who want to make an immediate difference, she said.
In the long run, Geisler said, the key lies in treating substance abuse from a medical perspective. Strategically placing treatment resources in the communities that need them, educating people and providers, and collaborating mental health and community-based resources takes time.
"If we come together and look at what we can do by pulling together resources, aligning activities, focusing on joint outcomes and holding each other responsible, we can move forward, and we can drive change in our community around some of these complex issues," she said.
"In the meantime, it doesn't stop the deaths."